Presbyopia
Myopia
Short sightedness. Occurs when light from a distant object focuses 'in front' of the retina. A concave lens (negative powered lens) is used to re-focus the light on to the retina.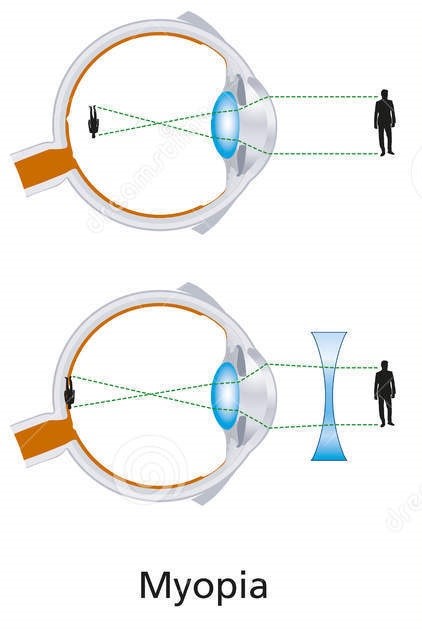
Hypermetropia (also known as Hyperopia)
Long sightedness. Occurs when light from a distant object focuses 'behind' the retina. A convex lens (positive powered lens) is used to re-focus the light on to the retina.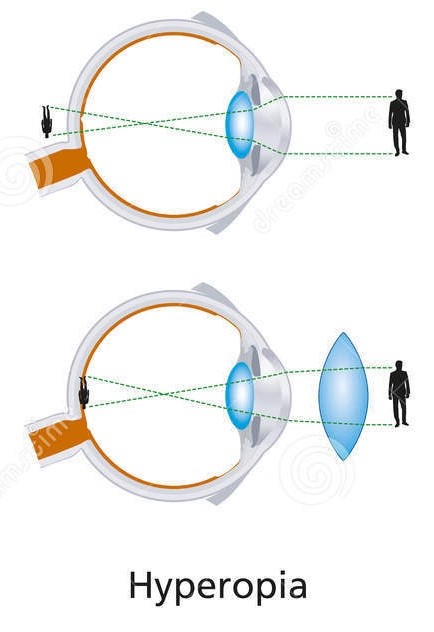
Astigmatism
Astigmatism is an optical defect in which vision is blurred due to the inability of the optics of the eye to focus a point object into a sharp focused image on the retina. This is corrected by incorporating an astigmatic lens with a concave or convex lens.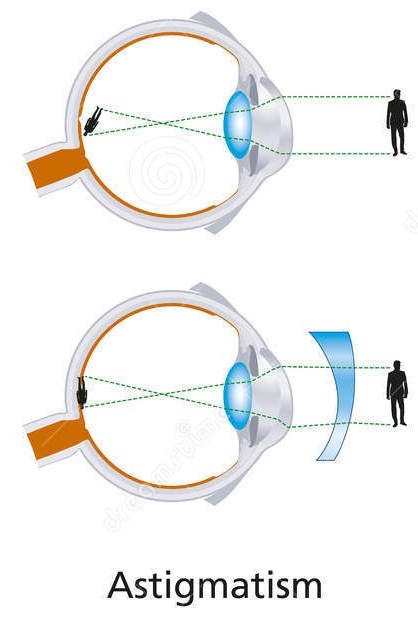
Cataracts
Cataracts are cloudy patches that develop in the lens of your eye.
A cataract is a clouding of the lens in your eye and can develop in one or both eyes. The lens is normally clear and sits behind the iris - the coloured part of the eye.
The lens helps focus light to produce a sharp image on to the retina at the back of the eye and changes shape to allow you to see close objects.
A cataract acts like a frosted glass coating that scatters light, causing blurring and lack of clarity.
Many studies are being carried out on cataracts, though no one knows exactly what causes them.
Factors that may be linked to causing cataracts include:
- Excessive exposure to sunlight
- Smoking
- Taking steroids for long periods of time
- Poor diet
- Injury
- Exposure to toxic materials and radiation
Cataracts can form at any age; there are cases where babies are born with them and they are known as congenital cataracts. In younger people they can result from conditions such as diabetes, certain medications and other eye problems. Cataracts normally occur as the eye gets older with many over 60's having them.
Cataracts are painless and usually cause a gradual worsening of sight. The main symptoms are:
- Blurring: Your vision may become misty or blurry so that you cannot see details at a distance, or your glasses seem scratched and dirty.
- Dazzled by lights: You may find that you have poor vision in bright light, suffer from glare, and that bright lights such as car headlights are more blinding than usual.
- Double vision: You may start to notice double vision for either close or distance objects.
- Changes in colour vision: You may notice that colours appear faded or washed out.
Some of these symptoms may be signs of other eye diseases. Your Optometrist will be able to use specialist equipment to monitor any changes in the lens that may lead to cataracts several years before any symptoms appear.
If you drive you must be able to reach the visual standards required; if you have a cataract this may need to be removed so that you can legally drive.
No prevention methods are proven, although 100% ultraviolet protection sunglasses are recommended.
If eligible for sugery, you will have a pre-operative assessment. The operation takes around 20 minutes and is carried out through a tiny cut in the eye that doesn't need stitches. You will have to use drops and wear a pad to protect the eye after surgery.
Vision is usually instantly improved, though healing may take several months. If you wear glasses you are more likely to need a new prescription, especially for reading as the intra-ocular lens is normally only set for distance vision.
We recommend that you have an Eye Test every two years, unless your Optometrist advises otherwise.
Glaucoma
Glaucoma is the name given to a group of eye conditions where the optic nerve is damaged at the point where it leaves the eye. The optic nerve carries images from the retina, the light sensitive membrane attached to the inner surface of the eye, to the brain.
There are four main types:
- Chronic glaucoma (slow onset)
- Acute glaucoma (sudden onset)
- Secondary glaucoma (caused by another eye condition)
- Congenital or developmental glaucoma (a condition in babies caused by malformation of the eye)
According to the RNIB, chronic glaucoma affects one percent of people over 40 and five percent of people over 65. The risk of glaucoma increases with age and if left untreated it can cause blindness.
For most people, there are usually few or no symptoms of glaucoma. The first sign of glaucoma is often the loss of peripheral or side vision, which can go unnoticed until late in the disease. This is why glaucoma is often called the 'sneak thief of vision.'
If you have any of the following symptoms, seek immediate medical care:
- Seeing halos around lights
- Vision loss
- Redness in the eye
- Eye that looks hazy (particularly in infants)
- Nausea or vomiting
- Pain in the eye
- Narrowing of vision (tunnel vision)
Glaucoma treatment may include prescription eye drops, laser surgery, or microsurgery.
Open-angle glaucoma is most commonly treated with various combinations of eye drops, laser trabeculoplasty, and microsurgery. Traditionally in the U.S., medications are used first, but there is increasing evidence that some people with glaucoma may respond better with early laser surgery or microsurgery.
Infant or congenital glaucoma -- meaning you are born with it -- is primarily treated with surgery, because the cause of the problem is a very distorted drainage system.
Flashes and Floaters
The eye is filled with a clear, jelly-like substance called the vitreous humour that helps maintain the eye's shape. Debris within the vitreous humour casts a shadow on the retina at the back of the eye, and appears to 'float' in your field of vision. Floaters can appear in a variety of shapes and sizes such as black dots, smoke, shadow or hairs. They are more visible against clear, pale backgrounds such as white walls or blue sky. They move when your eye moves in different directions and seem to dart away when you look at them.
Most floaters are small but larger floaters can be annoying and make activities that require higher concentration, such as reading or driving more difficult. Although most people naturally experience floaters, they are usually harmless. They can also be caused by a Posterior Vitreous Detachment (PVD) or a detachment or tear of the retina (the light sensitive tissue inside the eye). These can also cause symptoms of 'flashing lights'.
Changes in the vitreous humour occur over a lifetime. With age, strands of collagen start to become visible within the vitreous humour and it is the shadow of these strands that gives the sensation of floaters. Light travels through the clear layer of vitreous humour in order to reach the retina, which then transmits images to your brain via the optic nerve.
When you are young, the vitreous humour is attached to the retina, but it starts to shrink and change over time and can pull away from the retina-this is known as a PVD. A PVD can cause floaters and also “flashing lights” by pulling on and stimulating the retina. This causes your brain to interpret the pulling as a light signal which creates the sensation of “flashes”.
Floaters often occur in people over 40 as the eye gets older; but are most common in people in their 60s and 70s. People who are myopic (short-sighted) are more likely to experience floaters.
In some cases the vitreous humour can tear the retina as it pulls away. If the retina tears or detaches, blood can escape into the vitreous humour, causing a “shower” of floaters and flashes. Retinal tears or detachments may also be the result of causes such as impact to the head or eye
Many people do not notice floaters as the brain constantly adapts to changes in vision. However a sudden onset of floaters or flashing lights can indicate something more serious. The symptoms are never painful.
Consult an optometrist immediately if you:
- Notive a sudden increase in the number of flaters or they start to look different
- Start tos ee flashing lights
- Have experienced floaters in one eye but they now appear more noticable or appear in the other eye
- Have floaters which make it difficult to carry out everyday tasks, such as driving or reading
- Have a grey area, shadows, or hair-like areas appearing in your vision
Floaters do not usually cause long-term visual impairment; but you should tell your Optometrist if they occur.
The Optometrist will check your vision and examine the back of your eye using a microscope. Drops will enlarge the pupil giving the Optometrist a better view of the inside of the eye; and your peripheral vision may be checked using a visual fields analyser. If it is suspected that you have a retinal tear or detachment you will be referred to a hospital.
Eye drops will not make floaters disappear. If one appears in your line of vision, try moving your eye quickly up then down. This causes the vitreous humour to swirl about and move the floater else where.
If your floaters aren’t a sign of retinal damage, they may disappear, become less noticeable, or stay and become irritating.
We recommend that you have an Eye Test every two years, unless your Optometrist advises otherwise.
Macular Degeneration
The retina is the light sensitive membrane attached to the inner surface of the eye. Light enters the eye and falls on the retina allowing us to see images, these are transmitted along the optic nerve to the brain where they are processed so we can see.
The macula is a small area in the middle of the retina with the greatest amount of light sensitive cells and is used for fine – detailed central vision. Macular degeneration is a painless disorder that can effect either eye, causing progressive loss of central and detailed vision.
Age - Related Macular Degeneration (AMD) is the most common form, although some forms affect younger people. There are two main types of AMD, referred to as ‘wet’ and ‘dry’. This is not a description of how the eye feels, but of whether leaking blood vessels are involved. Dry AMD accounts for 90% of cases, with 10% being wet AMD. Dry AMD can become Wet AMD.
Wet AMD can cause a sudden onset of symptoms over days, resulting from a build up of fluid under the retina. Dry AMD progresses slowly over a no of years and the symptoms will onset gradually and includes blurred or absent central vision. Distortions can also occur so that straight lines appear wavy, or objects appear larger or smaller than normal, making it difficult to judge distances accurately. It may be difficult to read, recognise people, watch television and drive. However the peripheral vision remains clear and those with AMD can still move around fairly freely.
During your eye examination the optometrist may use a grid called an amsler grid to see if the grid appears distorted or missing or if there is a size difference that can be seen. If the degeneration is at an advanced stage then you will lose your central vision.
‘Wet’ AMD – Treatment is only effective if the AMD is detected early; this is essential as it can damage vision. Laser surgery to stem leaking blood vessels may be used, or repeated Photodynamic Therapy may be applied, where a laser is shone on the eye activating a medicine that destroys abnormal vessels. Other treatment advances include injections of anti-VEGF drugs such as Macugen directly into the eye.
‘Dry’ AMD – no treatment can prevent further degeneration.
Evidence show that increasing dietary antioxidants and carotenoids reduce the risk of AMD. Lutein and zeaxanthin are nutrients thought to help protect the macula; they are obtained from foods such as spinach, broccoli and sprouts which contain high levels. If you cannot increase your leafy green intake, supplements are available. Ask your optometrist to recommend some. For those with significant sight loss, magnifiers and high powered reading glasses can aid vision.
Diabetic Retinopathy
It occurs when high blood sugar levels damage the cells at the back of the eye.
Diabetic retinopathy is caused by prolonged high blood glucose levels. Over time, high sugar glucose levels can weaken and damage the small blood vessels within the retina.
This may cause haemorrhages, exudates and even swelling of the retina.
This then starves the retina of oxygen, and abnormal vessels may grow. Good blood glucose control helps to lower diabetes retinopathy risks
Like many conditions of this nature, the early stages of diabetic retinopathy may occur without symptoms and without pain. An actual influence on the vision will not occur until the disease advances.
Macular oedema can result from maculopathy and affect vision occurs if leaking fluid causes the macular to swell. New vessels on the retina can prompt bleeding, which can also block vision in some cases.
Symptoms may only become noticeable once the disease advances, but the typical symptoms of retinopathy to look out for include:
- Sudden changes in vision / blurred vision
- Eye floaters and spots
- Double vision
- Eye pain
Dry Eye
Dry eye is caused by a problem with the drainage, evaporation or production of tears
Dry eye is a common medical condition and is caused by a problem with the drainage, evaporation or production of tears. Tears are moved across the eye when you blink to lubricate the front surface of your eye, wash away debris, protect against infection and to help stabilise vision.
Tears are made up of three main components: an outer lipid layer which prevents tears from evaporating and eyelids from sticking together, a middle watery layer which carries nutrients and oxygen, and an inner mucous layer which allows the tears to wet the cornea. Each layer is produced by different glands in and around the eyelids.
It is possible to be diagnosed with dry eye even if you have very watery eyes; this can be due to a problem with one of the other layers of the tears. Dry eye can usually be easily managed.
Dry eye syndrome can occur if your eyes do not produce enough tears or tears evaporate too quickly. There are many different reasons why this can happen, although a single identifiable cause is not often found. Hormones stimulate the production of tears. Changes in hormone levels in women (for example during the menopause or pregnancy or while using the contraceptive pill) can increase their risk of dry eye.
Dry eye syndrome is more common in older people, possibly because you produce fewer tears as you get older and your eyelids become less effective at spreading tears over your eyes. Environmental factors can have a drying effect on your eyes, causing your tears to evaporate. These include sun, wind, dry climate, hot blowing air and high altitude.
Your Optometrist will offer treatment advice. Failure to treat dry eye may result in complications such as damage to the cornea.
Blepharitis
Blepharitis is the inflammation of the eyelids. There are two types:
- Anterior blepharitis - this affects the area of the eyelids where the eyelashes sit.
- Posterior blepharitis - this affects the meibomian glands which produce part of the tears.
Blepharitis is common and GPs say it accounts for 5% of all eye problems they see.
For many people blepharitis is often a low level, but chronic inflammation and many experience periods of time when there are no symptoms. However, inflammation can occur for long periods of time and may require treatment. While blepharitis can be quite uncomfortable, it is not usually a serious condition and vision is seldom affected. Blepharitis can also cause problems with the consistency of the tears which may lead to dry eye symptoms.
Your Optometrist or doctor can spot the signs of blepharitis by looking closely at your eyelids.
Eyelid hygiene is the first line of management:
- Use a dedicated lid cleaning solution for the best results(e.g. Blephasol/Blephaclean). Apply as per the instructions. This usually involves applying the solution on a swab to the lid margin area for 2-3 minutes which cleans the lids and lashes, wiping away bacteria. Do not clean the inside of the eyelids as this can damage the eye.
- Then use slight pressure with the swab to massag the eyelids starting away from the edge of the lids and rolling towards the lid margins to expel excess fluid from the eyelid glands.
- Warm compresses/masks pressed against the eyelids can help loosen crusts and soften the waxy build up from within the glands.
- Avoid using eye make up (mascara and eyeliner particularly) until symptoms have cleared. This makeup will need replacing when the infection has cleared to avoid contamination.
- Severe cases may need antibiotics or tear supplements.
Your Optometrist will be able to give you advice on the most suitable products to use. Avoid sharing towels as the infection can be passed on
Conjunctivitis
Conjunctivitis is a condition that is often referred to as red eye.
Conjunctivitis is a common condition that causes redness and inflammation of the thin layer of tissue that covers the front of the eye (the conjunctiva).
People often refer to conjunctivitis as red eye
The conjunctiva can become inflamed as result of:
- a bacterial or viral infection – this is known as infective conjunctivitis
- an allergic reaction to a substance such as pollen or dust mites – this is known as allergic conjunctivitis
- the eye coming into contact with substances that can irritate the conjunctiva, such as chlorinated water or shampoo, or a loose eyelash rubbing against the eye – this is known as irritant conjunctivitis
Symptoms of conjunctivitis include itchiness and watering of the eyes, and sometimes a sticky coating on the eyelashes (if it's caused by an allergy).
Conjunctivitis can affect one eye at first, but usually affects both eyes after a few hours
Conjunctivitis often doesn't require treatment as the symptoms usually clear up within a couple of weeks. If treatment is necessary, the type of treatment will depend on the cause. In severe cases, antibiotic eye drops can be used to clear the infection.
Irritant conjunctivitis will clear up as soon as whatever is causing it is removed.
Allergic conjunctivitis can usually be treated with anti-allergy medications such as antihistamines. If possible, avoid the substance that triggered the allergy.
It's best not to wear contact lenses until the symptoms have cleared up. Any sticky or crusty coating on the eyelids or lashes can be cleansed with cotton wool and water.
Washing your hands regularly and avoiding sharing pillows or towels will help prevent it spreading.
See your GP immediately if you have:
- Eye pain
- sensitivity to light (photophobia)
- Disturbed vision
- intense redness in one or both of your eyes
